ACS Multimedia Atlas of Surgery: Colorectal Surgery Volume
Editors: Horacio J. Asbun, MD, FACS; Tonia M. Young-Fadok, MD, MS, FACS, FASCRS

| Product Details | |
| Year Produced: | 2008 |
| Pages: | 235 |
| Dimensions: | 8.5x11 in |
| ISBN: | 978-1-880696-36-1 |
Includes book with full online access to all chapters. Price includes shipping costs.
For assistance, comments, or questions, contact Olivier Petinaux, Senior Manager, Distance Education and E-Learning, elearning@facs.org or call us at 1-866-475-4696
The American College of Surgeons Division of Education and Ciné-Med have developed the interactive Multimedia Atlas of Surgery: Colorectal Surgery Volume.
A comprehensive atlas style text, this volume includes 26 chapters presenting open and laparoscopic surgical techniques for treating colorectal disorders. Expert surgeons provide detailed, step-by-step instruction using a combination of video, illustration, and intraoperative photos to clarify specific points of the procedure.
From diagnostic procedures to total resections for cancer, this atlas provides in-depth instruction on procedures of or relating to the colon and rectum.
Procedures:
- Colonoscopy
- Colostomy
- Colectomy
- Hemicolectomy
- Sigmoid Colectomy
- Low Anterior Resection
- Ileoanal Anastomosis
- Abdominoperineal Resection
- Bowel Strictureplasties
- MACE Procedure (Malone Antegrade Continence Enema)
Individual titles are available for purchase. Select one below.
- Colonoscopy: Diagnostic
Kenneth A. Forde, MD, FACS - Colonoscopy: Therapeutic
Kenneth A. Forde, MD, FACS - Laparoscopic Appendectomy
Klaus Thaler, MD, FACS - Laparoscopic Creation of Colostomy and Ileostomy
Eric J. Dozois, MD, FACS, FASCRS - Laparoscopic Colostomy Takedown/Reversal of Hartmann's Procedure
B. Todd Heniford, MD, FACS - Laparoscopic Right Colectomy
Jonathan E. Efron, MD, FACS; Joseph W. Nunoo-Mensah, BMed Sci, BMBS, FRCS (Eng), LLM - Right Hemicolectomy with Intracorporeal Anastomosis
Morris E. Franklin, Jr., MD, FACS; Jorge M. Trevino, MD - Laparoscopic Sigmoid Colectomy: Lateral-to-Medial Approach
Conor P. Delaney, MBBCh, PhD, FACS; Michael S. Wolfe, MD - A Standardized Technique for Medial-to-Lateral Laparoscopic Sigmoid Colectomy
Anthony J. Senagore, MD, MS, MBA, FACS - Laparoscopic Low Anterior Resection for Rectal Cancer with Specific Focus on Nerve Preservation
Jacques Marescaux, MD, FRCS, FACS, FRCS; Joel Jules Louis Leroy, MD, FRCS; Charles Bailey, MD, FRCS - Hand Assisted Laparoscopic Total Colectomy and Ileorectal Anastomosis
James W. Fleshman, MD, FACS - Laparoscopic Proctocolectomy and Brooke Ileostomy
David Vivas, MD; Marat Khaikin, MD; Steven D. Wexner, MD, FACS - Laparoscopic Proctocolectomy and Ileal-Pouch Anal Anastomosis (IPAA)
Tonia M. Young-Fadok, MD, MS, FACS, FASCRS; Joseph W. Nunoo-Mensah, BMed Sci, BMBS, FRCS (Eng), LLM - Hand Assisted Laparoscopic Proctocolectomy with Ileoanal Pouch (IPAA)
Peter W. Marcello, MD, FACS - Laparoscopic Abdomino-perineal Resection
Matthew G. Mutch, MD, FACS - Laparoscopic Rectopexy for Rectal Prolapse
Sergio W. Larach, MD, FACS - Laparoscopic Assisted Pull-through for Imperforate Anus
Steven S. Rothenberg, MD, FACS - Transanal Endoscopic Microsurgery Procedure for Low Rectal Tumors
Gerhard Buess, MD, FRCS; Mark H. Whiteford, MD, FACS; Lee L. Swanstrom, MD, FACS - Open Right Hemicolectomy
Luca Stocchi, MD - Open Sigmoid Colectomy
Richard P. Billingham, MD, FACS - Open Total Mesorectal Excision and Coloanal Anastomosis
Professor R J Heald, OBE, MChir, FRCS - Open Proctocolectomy and Ileal-Pouch Anal Anastomosis (IPAA)
John H. Pemberton, MD, FACS, FASCRS; Robert R. Cima, MD, FACS, FASCRS - Full Thickness Transanal Approach for Low Rectal Tumors
John H. Marks, MD, FACS, FASCRS - Open Abdomino-perineal Resection
Robert D. Madoff, MD, FACS; Gonzalo Hagerman, MD - Bowel Strictureplasties
Fabrizio Michelassi, MD, FACS
Richard P. Billingham, MD, FACS
Professor Gerhard F. Buess, MD, FRCS
Robert R. Cima, MD, FACS, FASCRS
Jose R. Cintron, MD, FACS
Conor P. Delaney, MD, PhD, FACS
Eric J. Dozois, MD, FACS, FASCRS
Jonathan E. Efron, MD, FACS
James W. Fleshman, MD, FACS
Kenneth A. Forde, MD, FACS
Morris E. Franklin, Jr., MD, FACS
Gonzalo Hagerman, MD
Professor R J Heald, OBE, MChir, FRCS
B. Todd Heniford, MD, FACS
Marat Khaikin, MD
Sergio W. Larach, MD, FACS
Joel Jules Louis Leroy, MD, FRCS
Robert Madoff, MD, FACS
Peter W. Marcello, MD, FACS
Jacques Marescaux, MD, FR CS, FACS
John H. Marks, MD, FACS, FASCRS
Fabrizio Michelassi, MD, FACS
Matthew Mutch, MD, FACS
Richard Nelson, MD, FACS
Joseph W. Nunoo-Mensah, BMed Sci, BMBS, FRCS (Eng), LLM
John H. Pemberton, MD, FACS, FASCRS
Madeleine Poirier, MDCM, MSc, FRCSC, FACS
Steven S. Rothenberg, MD, FACS
Anthony J. Senagore, MD, MS, MBA, FACS, FASCRS
Luca Stocchi, MD
Lee L. Swanstrom, MD, FACS
Klaus Thaler, MD, FACS
Jorge M. Trevino, MD
David Vivas, MD
Steven D. Wexner, MD, FACS
Mark H. Whiteford, MD, FACS
Michael S. Wolfe, MD
Tonia M. Young-Fadok, MD, FACS, FASCRS
With the many imaging methods available for evaluation and often therapy of colorectal disorders, colonoscopy has emerged as the gold standard for diagnosis. It is also, in some areas, an increasingly frequent option for therapy, be it definitive or palliative.

Preparation for colonoscopy, of a necessity, should include preparation of the endoscopist, preparation of the patient in general and of the colon specifically. Before starting a diagnostic procedure it is necessary to ensure that the instrument to be used is in working order, that air, water and suction channels are operating properly, that biopsy forceps, cytology brush, snare and cautery devices are available.

If fluoroscopy is available, the overtube (external splinting device) is placed over the colonoscope before initiating the examination.

An intravenous line is inserted, fluids started and pre-procedure antibiotics administered if indicated. While the use of pulse oximetry and intermittent monitoring of blood pressure as well as electrocardiography (if clinically indicated) have now become standard procedures, it is important for the assistant as well as the endoscopist to be aware of any changes in the patient's level of awareness, respiration and abdominal distention.

The main objective on insertion of the instrument is to reach the most proximal point desired in as expeditiously a fashion as possible, leaving detailed inspection until the process of withdrawal of the endoscope. The examiner must appreciate that the colon is of variable length, that respiratory and peristaltic activity is in progress during the examination and that some areas of the colon are more fixed (by normal anatomy, previous inflammation or postoperative change). It is dangerous to proceed with introduction of the endoscope without knowing at all times the location of the lumen.
Proctocolectomy and ileal pouch-anal anastomosis (IPAA) is one of the most complex of colorectal procedures. A minimally invasive approach adds further technical complexity. We have addressed initial concerns regarding complexity by developing a simplified technique. This technique utilizes the anatomy of the colon and rectum, which become midline structures, centered in the mid-abdomen, once they have been fully mobilized and the distal rectum is transected.

The simplified procedure may be broken down into 5 main steps. Each step is completed before moving to the next step in order to minimize position changes and be efficient. Following trocar placement and abdominal exploration, Step 1 involves mobilization of the left colon. In Step 2 the right colon is mobilized. Laparoscopic pelvic dissection with full mobilization of the rectum and transection at the pelvic floor is performed in Step 3. In Step 4 exteriorization, resection and pouch creation are performed via a 4-5 cm periumbilical incision. Step 5 is creation of the laparoscopic ileal pouch-anal anastomosis and formation of a loop ileostomy.
IPAA is most commonly performed for ulcerative colitis and familial adenomatous polyposis. The goal of surgical intervention is to eradicate disease and restore intestinal continuity. The extent of the resection, plus the reconstruction, results in this being one of the most complex colorectal surgical procedures. Frequent coexistence of inflamed bowel, malnutrition and immunosuppression add to the complexity.
The issue of complexity has been addressed, by simplifying the procedure wherever possible and by building on the lessons learned from the simplification of segmental procedures. Our technique has evolved to: a four port technique, lateral-to-medial dissection of the right and left colon, intracorporeal mobilization of the rectum, 4-5 cm extension of the supraumbilical port site incision around the umbilicus for specimen extraction, and use of the right lower quadrant port site for the ileostomy.
The indications for operative intervention in UC are not changed by the laparoscopic approach. Thus surgical management is appropriate for UC refractory to medical therapy; side effects from medical therapy; development of dysplasia or malignancy, and (in pediatric patients) growth retardation. A laparoscopic approach may be feasible in selected cases of emergent presentations of UC including perforation with minimal contamination and a stable patient, toxic megacolon and bleeding. In the setting of UC-associated dysplasia or malignancy, or FAP with malignancy, an oncologic resection is required and the specifics for these indications will be addressed with the relevant steps.
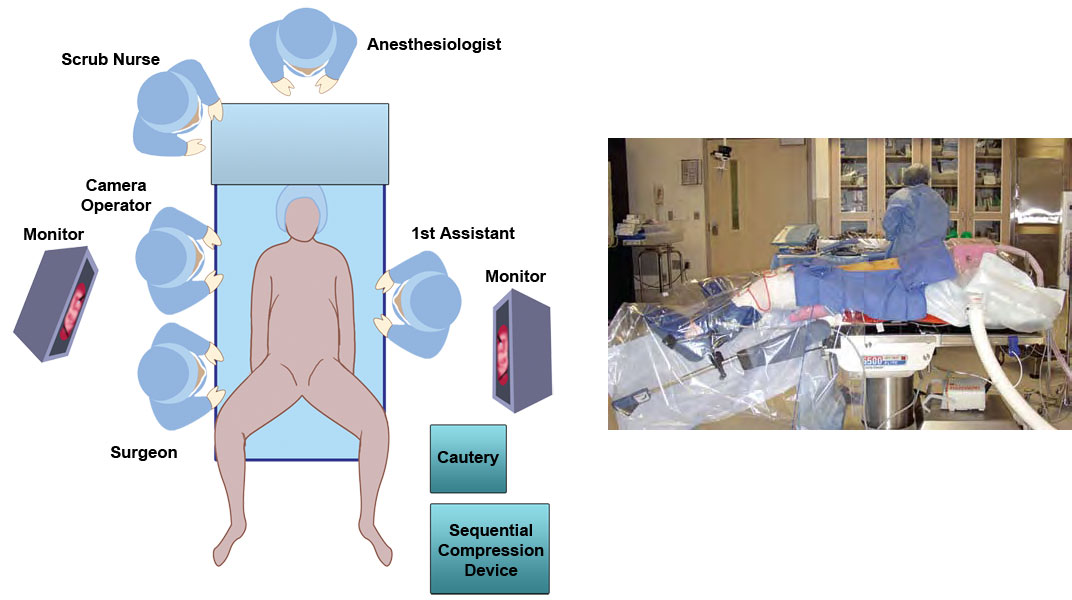
The patient lies on the operating table on "egg-crate" foam that is taped to the table, to prevent slipping during steep position changes. The patient's distal sacrum is positioned at the end of the table to allow access for mucosectomy or a circular stapler. The legs are placed in Lloyd-Davies stirrups, with the thighs parallel to the abdomen to prevent interference with instruments in the lower quadrant ports. The patient's hands are protected with foam padding and the arms tucked beside them with a sheet placed under the patient, wrapped around the arms and folded beneath the torso. Additional foam padding is laid on the patient's chest before securing the upper body with a chest strap. A bladder catheter, orogastric tube, and sequential compression devices are placed.
Sufficient room must be preserved around the operating table to allow monitors to be moved between the level of the patient's shoulders and ankles, in line with the surgeon's field of view, as work proceeds in different quadrants of the abdomen and in the pelvis. The laparoscopic tubing and leads are placed on the OR table and checked. The laparoscopic tower containing the light source, camera and insufflator are positioned on either right or left side to produce minimum interference with table changes and surgeon movement depending on configuration of the operating room.



